Bridges-2 Image Processing Gives AIs a Leg Up on Better, Faster Help for People with Mental Disorders
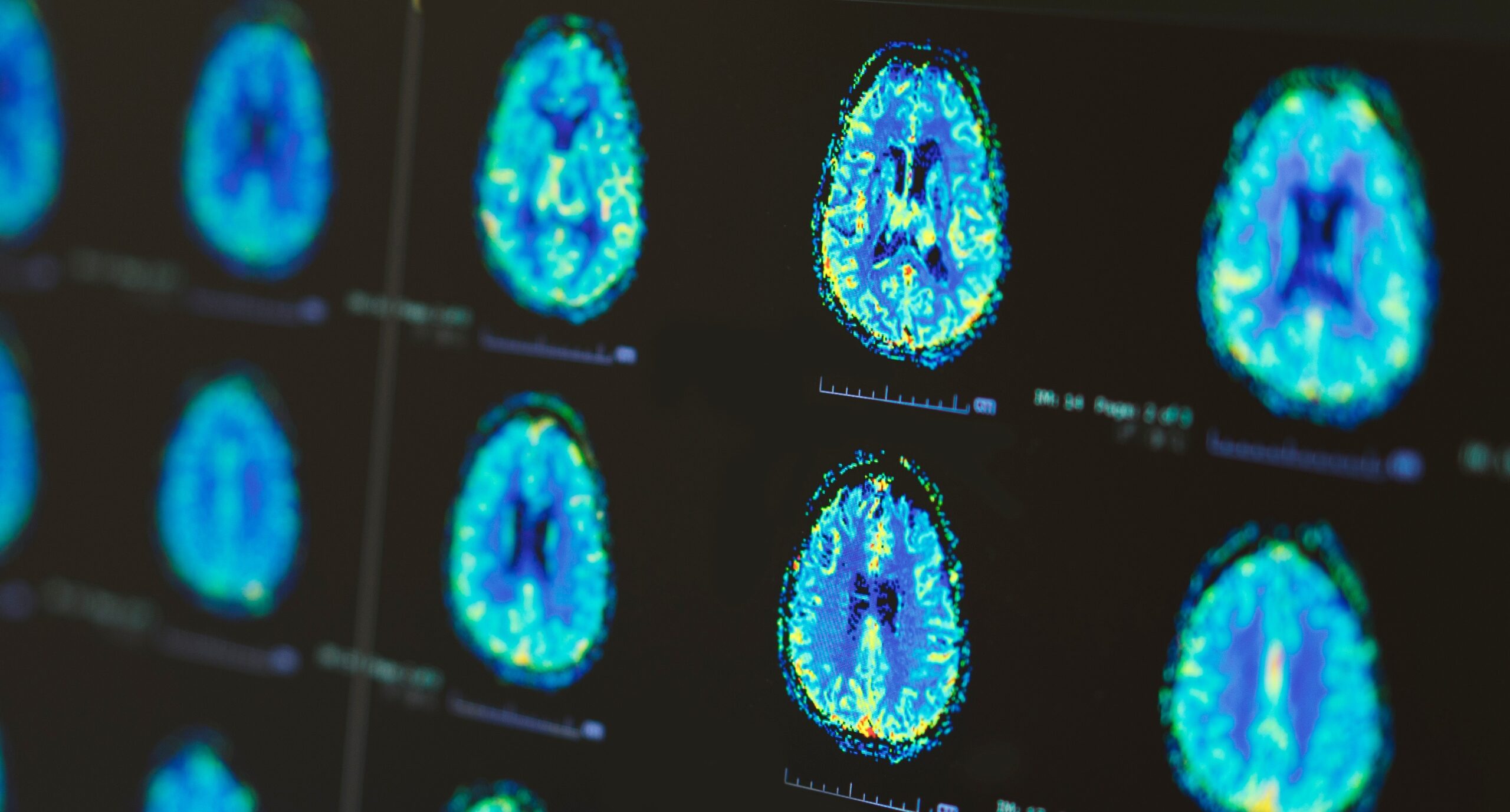
Psychiatric illnesses are defined by clusters of symptoms. But those symptoms overlap a lot between different disorders, posing problems both for diagnosis and proper treatment. A team from the University of Pittsburgh used PSC’s NSF-funded Bridges-2 and artificial intelligence to analyze brain scans of people with different disorders, as well as people without psychiatric issues. Their AI tools improved on diagnostic accuracy over human experts, offering the hope of more reliable diagnosis and appropriate treatment.
WHY IT’S IMPORTANT
The field of psychiatry offers at least partial help to many people with mental disorders. But not all patients recover completely.
One problem is that the clinical manual for psychiatric diagnosis, the Diagnostic and Statistical Manual of Mental Disorders, defines and categorizes psychiatric illnesses imperfectly. Psych diagnoses are chiefly defined by clusters of symptoms occurring together more often than can be explained by chance. But these symptoms overlap between disorders. For example, hallucinations can appear in major depressive disorder, bipolar disorder, or schizophrenia.
“The issue with psychiatric diagnoses is that they are basically clusters of symptoms that tend to occur together … The trouble with that kind of definition is that there are no specific symptoms for most disorders. So we cannot say, OK, if this symptom occurs, this is the diagnosis, because the same symptom can occur in multiple disorders.
— Konasale Prasad, University of Pittsburgh
Diagnoses of the same patient can differ between psychiatrists, or even the same psychiatrist at different times. And how all the above connects with the biology of what’s happening in the brain isn’t clear. All of that’s a barrier to accurate diagnosis and effective treatment.
Ultimately, psychiatric disorders arise from activity in the brain. But the incredibly complicated pathways of nerve cell activity aren’t easy for the human eye to understand without help. University of Pittsburgh psychiatrist Konasale Prasad and his team wondered whether an AI tool could distinguish between the brain scans of people with different disorders better than experts. They approached this problem via an allocation on PSC’s flagship Bridges-2 system from ACCESS, the NSF network of supercomputing centers, in which PSC is a leading member.
HOW PSC HELPED
Previous work applying AI to psychiatric diagnosis had been encouraging, offering more accuracy and consistency over time than traditional diagnosis. As part of their ongoing investigations, Prasad and students decided to tackle an even more challenging problem: psychotic-like experiences (PLE).
People with PLE experience symptoms that are mild enough that they often don’t seek treatment. Their brain activity looks normal to the human eye. But adults with PLE are four times more likely to develop schizophrenia, major depressive disorder, or bipolar disorder during their lifetimes. Children with PLE are between five and 16 times more likely to develop mental illness.
The Pitt scientists used two types of AI, support vector machines (SVMs) and graph convolutional networks (GCNs), testing the effectiveness of each type. They trained their AIs using data from the UK Biobank, a national lifestyle and health data set that included data from 40,000 people with and without mental disorders. These folks had had three different types of brain MRI scans done, showing different aspects of brain activity.
The team fed their AIs a sampling of the MRI data from a group of people who had PLE; a group who had one of a family of illnesses known as psychosis spectrum disorders (PSD); and a third group who developed either schizophrenia, major depressive disorder, or bipolar disorder. They compared those groups to MRI data from people without psychiatric illness. This training data set had the “right answers” labeled. This allowed the AIs to make millions of comparisons, weeding out the ones that didn’t help it identify the correct disorder. The scientists then tested their AIs using data without the answers labeled, to see how accurate it was without the cheat sheet.
Splitting the brain scans into a manageable number of chunks that were still small enough for the computer to make good comparisons would take a lot of computation. The image-friendly graphics processing units (GPUs) in Bridges-2’s GPU nodes, with access to between 128 and 2,000 gigabytes of memory per node, offered the ability to carry out these computations on multiple brain scans at the same time, speeding the work greatly.
“We parcellate … the brain into a little over 360 small regions, which are structurally, functionally connected. That parcellation takes a very long time. When I first started doing those parcellations … it was only doing about 65 or 66 different regions. It used to take one full day, 24 hours, on my workstation. But on Bridges-2, we can get it done in about six hours, and we can feed multiple MRI scans, where it parallelizes, processes and then gives out the results. So we can get to the actual analysis very quickly.”
— Konasale Prasad, University of Pittsburgh
The results encouraged the Pitt scientists. The best of the AIs showed accuracies above 65 to 70 percent. That accuracy would need to be better before being applied to real patients. But given that psychiatrists’ accuracy for these diagnoses of PLE is between 35 and 40 percent, the AIs are clearly on the right track. The team reported these results in the journal Neural Networks in September 2024. Using the same AI models on a group of adolescent schizophrenia patients, the best AIs were 90 percent accurate, compared with professionals’ roughly 65 percent accuracy. To improve reproducibility with different atlases, they reported methods to reconcile these differences, in the Journal of Neuroscience Methods, April 2025.
Prasad would like to expand the work to more GPU nodes, allowing his team to analyze more brain scans faster, and in finer detail. That work is ongoing. He’d also like to look at finer distinctions between different types of psychiatric disorders, and to grapple with the difficult call of when a given patient is more likely to be at risk of suicide or aggression toward other people, a task professionals currently struggle with.
